DHHS → MeCDC → Disease Surveillance → Epidemiology → Airborne and Direct Contact Diseases → Coronavirus → Long-Term Care and Other Congregate Living Facilities
COVID-19: Long-Term Care and Other Congregate Living Facilities
Due to the number of individuals living in close proximity to one another, long-term care facilities and other congregate living facilities are at high risk of being affected by Novel Coronavirus 2019 (COVID-19).
On this page:
- COVID-19 Positive in the Facility
- Personal Protective Equipment (PPE)
- Prevention
- Reporting COVID-19 Cases
- Outbreaks and Universal Testing
- Webinars and Other Presentations
- Additional Resources
COVID-19 Positive in the Facility
- Visit Maine CDC's Healthcare Associated Infections Program for information on responding to COVID-19 positives in a healthcare setting.
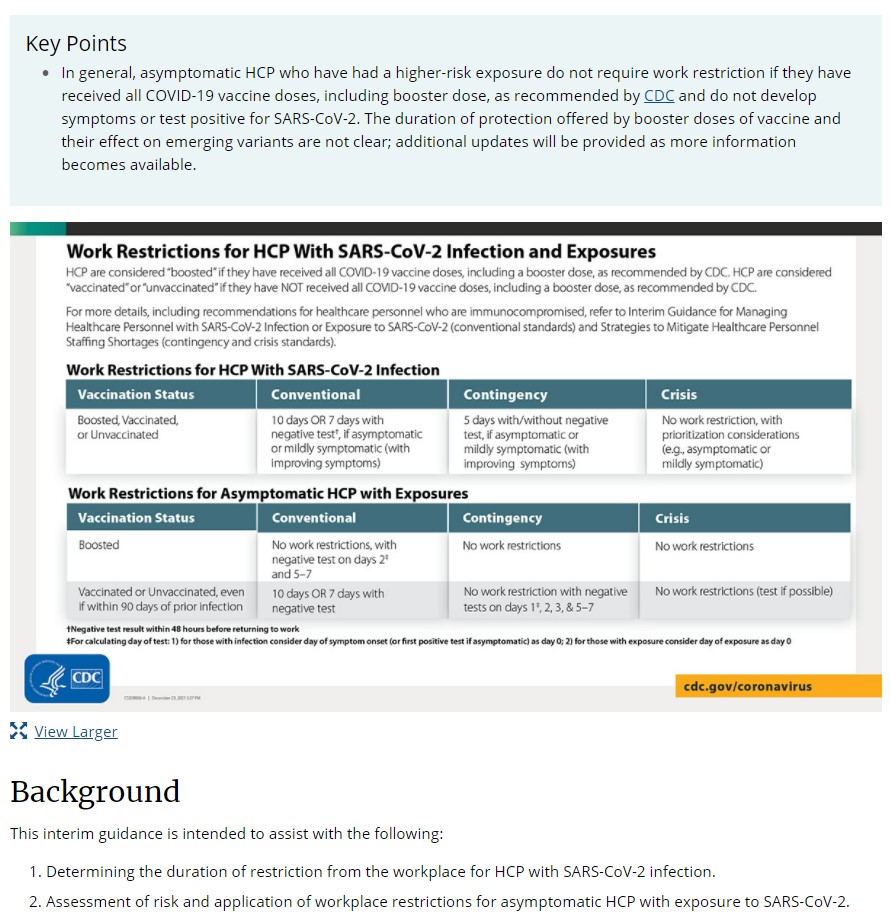
- Visit Interim Guidance for Managing Healthcare Personnel with SARS-CoV-2 Infection or Exposure.
- Visit Infection Prevention in Long-Term Care Facilities.
Personal Protective Equipment (PPE)
- Healthcare personnel should wear a facemask at all times when they are in the facility. When available, facemasks should be worn instead of cloth face coverings. Guidance on extended use and reuse of fasemasks is available. When PPE is required, for example when collecting a naspharyngeal swab (NP), cloth face coverings should NOT be worn by a healthcare provider instead of a respirator or facemask.
- Residents should wear a cloth face covering or facemask (if tolerated) whenever they leave their room, including for procedures outside the facility. Cloth face coverings should not be placed on anyone who has trouble breathing, or anyone who is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.
- Visitors, if allowed, should wear a cloth face covering while in the facility.
- Patients with confirmed or possible SARS-CoV-2 infection should wear a facemask when being evaluated medically. Healthcare personnel should adhere to Standard and Transmission-Based Precautions when caring for patients with SARS-CoV-2 infection.
If you are a facility in need of additional PPE, please start by using your normal channels to order PPE. If you cannot secure PPE through your normal channels, please reach out to your County Emergency Management Agency (EMA).
Prevention
Facilities should proactively implement infection prevention strategies and practices. This includes:
- Screening staff at the beginning of their shift for symptoms of COVID-19
- Screening residents
- Enhancing evironmental cleaning and disinfection
- Implementing visitor restrictions
- Adhering to a masking policy for staff, visitors, and residents leaving their rooms
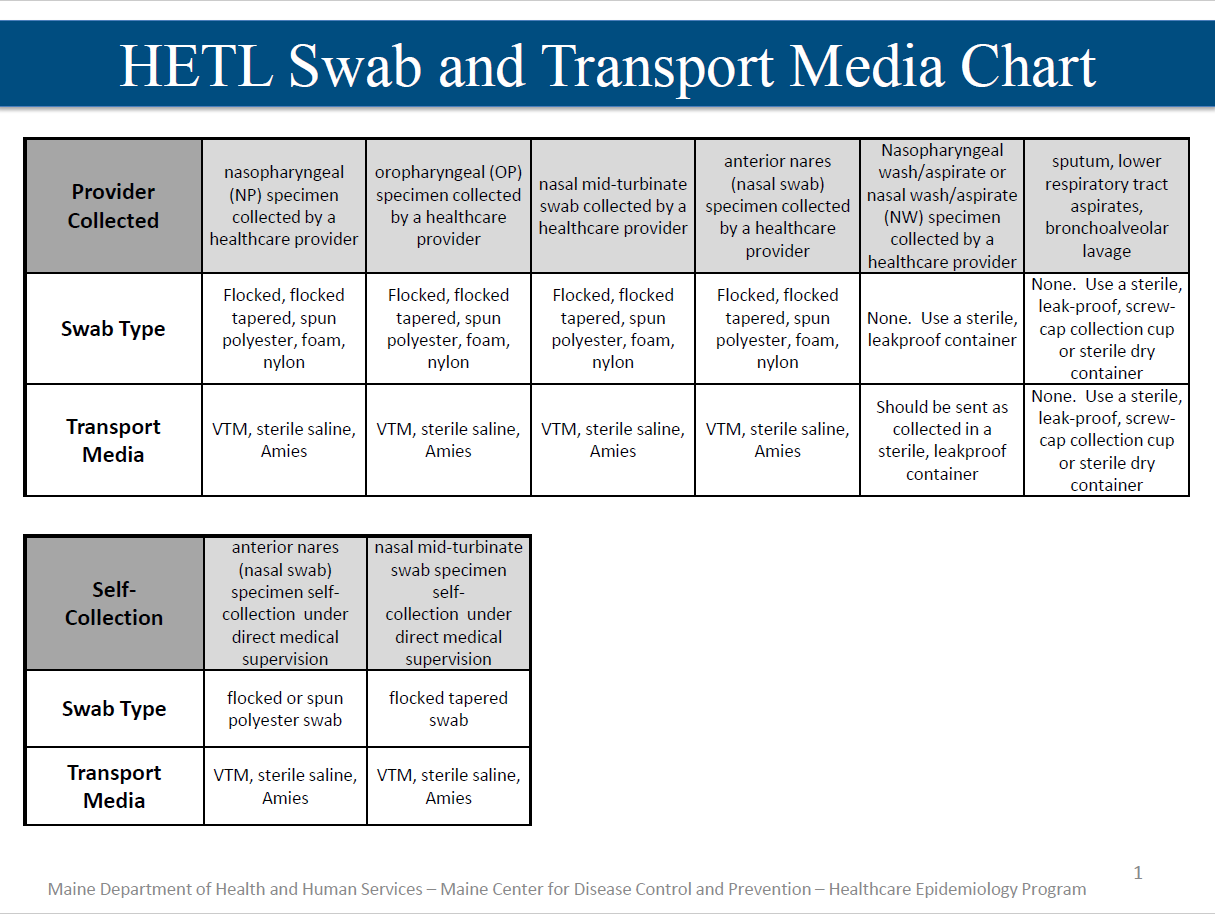
- Creating a testing plan in the event of symptomatic residents or staff, including identifying a healthcare provider that can perform specimen collection if necessary
- Implementing a sick leave policy
- Creating a plan for managing new admission and readmissions
- Implementing social distancing measures
Reporting COVID-19 Cases
Administrators and healthcare providers are required to report notifiable diseases and conditions, including COVID-19. This means that the laboratory as well as the facility should report a positive lab result to Maine CDC. Facilities should notify Maine CDC of a positive lab result by:
- Reporting results electronically through the online reporting system. To register and report results, follow these instructions (PDF) OR
- Calling Maine CDC at 1-800-821-5821 OR
- Faxing a completed case report form (PDF) to 1-800-293-7534
COVID-19 deaths are also required to be reported to Maine CDC.
Patients Under Investigation (PUIs), or suspect cases, do not need to be reported to Maine CDC unless their lab results come back positive.
Outbreaks and Universal Testing
Outbreaks of COVID-19 in congregate care facilities are defined as five cases or more within a fourteen day period. This may include both residents as well as staff.
When a congregate living setting has a single case of confirmed COVID-19 among staff or residents, Maine CDC recommends universal testing for all other staff and residents in the unit or building. Universal testing in this context refers to testing done by unit or building, not at a facility level, unless staff are shared or rotate among various units or buildings.
For more details, please see the Health Alert Network Advisory from May 23, 2020 (PDF).