Smoke Free City
Smoke Free City
Breaking up with tobacco is the #1 best thing you can do, and ChallengeME has a number of proven strategies to make quitting easier — even a smart phone app that tracks money saved and life expectancy added.
- Tobacco Cessation Resources
- Quitting Smokeless Tobacco
- Cessation and Therapy Info
Tobacco Cessation Program
Screening and Counseling Services:
- 2020 Expanded Maine Tobacco HelpLine Services (PDF)
- Lung Cancer Screening (age 55+) In Network 100% - no deductible Out of Network 60% after deductible
- Tobacco Use- In Network 100% - no deductible Out of Network- Not Covered
| Program | Who Is Eligible | Highlights |
|---|---|---|
|
Anthem: 1-844-273-4614 Pharmacy Benefit Manager- Medimpact 888-672-7151 888-672-7151 dial 711 for TTY - 24/7 |
Members of the Plan |
1. Physician visits for education and counseling related to tobacco use disorder. A counseling visit with one’s physician for Smoking and Tobacco Use Cessation with the appropriate coding can be covered at 100% with an in network provider. Out of network is subject to the out of network deductible and coinsurance. 2. Lung screening - a low dose CT scan is available for members 55 to 80 who have a history of smoking 30 packs per year and still smoke, or quit within the past 15 years. With the appropriate coding this will be covered at 100% with an In network provider. Out of network is subject to the out of network deductible and coinsurance. Since this is a CT scan, this will require a preauthorization to make sure the member meets medical necessity requirements. The plan also provides benefits for completing an approved smoking cessation program. We recommend the member consult with their primary care physician on the program/classes that are available. Smoking cessation classes are covered at 100% with an in network provider. Out of network is subject to the out of network deductible and coinsurance. |
|
1-844-207-LINK (5465) Available 24/7 |
Visit the Living Resources Program website for a complete list of covered employees/retirees. |
Provides short-term counseling with a licensed mental health provider. In addition, legal anf financial information and support, work-life solutions, back to school support, wellness coaching and online will preparation support |
|
(207)620-9202 sign into wellstarme.org and go to the "Resource Hub" |
Members of the State of Maine Health Plan |
Provides easy access to a variety of wellness programs including tobacco cessation. |
|
1-800-207-1230 |
Everyone |
Free Confidential Offers positive and supportive messages Offers personal support geared to your life All done by phone |
|
American Cancer Society |
Everyone |
Guide to Quitting Smoking What are the Benefits of Quitting? Desktop Helpers Resources and Tools ...and MUCH more! |
|
Centers for Disease Control and Prevention 1-800-QUIT-NOW (1-800-784-8669) |
Everyone |
Call for free help Read the Quit Guide Sign up for free texts to get free quit help texted to your phone |
|
Be Tobacco Free - FDA tobacco-free information |
Everyone |
Get on the path to a healthier you! Learn about the health benefits if you quit smoking right now. |
|
American Lung Association; Freedom From Smoking Program 1-800-LUNG-USA (1-800-586-4872) |
Everyone |
Designed for adults who are ready to quit smoking Small group counseling sessions Also offers an online program |
- The National Toxicology Program of the National Institutes of Health continues to classify smokeless tobacco as a known human carcinogen—proven to cause cancer in people. – US Surgeon General Richard Carmona, MD, MPH
- Smokeless tobacco is less lethal than cigarettes for most people, but using any form of tobacco puts you at serious health risks.
- All forms of oral tobacco have chemicals that cause cancer (carcinogens). These products can cause cancer of the mouth, throat, pancreas, and esophagus (the tube that carries food from the mouth to the stomach). Oral and smokeless tobacco also cause many other health problems, such as gum disease, destruction of the bone sockets around the teeth, and tooth loss. They cause bad breath and stained teeth, too.
- Smokeless tobacco products are called by a lot of names: Oral tobacco, chewing, snuff, snus, spit, spitless tobacco, and dissolvable nicotine, to name a few. (See Smokeless Tobacco for more details.) No matter what it’s called, smokeless tobacco is not a safe alternative to smoking. The bottom line: All forms of tobacco can be deadly.
Maybe you’ve tried to quit smokeless tobacco before. Why is quitting and staying quit so hard for so many people? The answer is mainly nicotine.
Nicotine
- Nicotine is a drug found naturally in tobacco, which is as addictive as heroin or cocaine. Over time, a person becomes physically dependent on and emotionally addicted to nicotine. The physical dependence causes unpleasant withdrawal symptoms when you try to quit. The emotional and mental dependence (addiction) make it hard to stay away from nicotine after you quit. Studies have shown that tobacco users must deal with both the physical and mental dependence to quit and stay quit.
Where nicotine goes and how long it stays
- Nicotine enters the bloodstream from the mouth or nose and is carried to every part of your body. It affects many parts of the body, including your heart and blood vessels, your hormones, the way your body uses food (your metabolism), and your brain. During pregnancy, nicotine freely crosses the placenta and has been found in amniotic fluid and the umbilical cord blood of newborn infants.
- Different factors affect how quickly the body gets rid of nicotine and its by-products. Regular oral tobacco users will still have nicotine and/or its by-products, such as cotinine, in their bodies for about 3 or 4 days after stopping.
How nicotine hooks tobacco users
- Nicotine causes pleasant feelings and distracts the user from unpleasant feelings. This makes the tobacco user want to use more. Nicotine also acts as a kind of depressant by interfering with the flow of information between nerve cells.
- As the nervous system adapts to nicotine, tobacco users tend to increase the amount of tobacco they use. This raises the amount of nicotine in their blood, and more tobacco is needed to get the same effect. This is called tolerance. Over time, the tobacco user reaches a certain nicotine level and then will need to keep up the usage to keep the level of nicotine within a comfortable range.
- Soon after a person finishes their dip or chew, the nicotine level in the body starts to drop, going lower and lower. The pleasant feelings wear off, and soon the user starts wanting more tobacco. If they delay using it, the person may start to feel irritated and edgy. Usually it doesn’t reach the point of serious withdrawal symptoms, but the tobacco user gets more uncomfortable over time. At some point, the person uses tobacco, the unpleasant feelings go away, and the cycle continues.
- Smokeless tobacco delivers a high dose of nicotine. Blood levels of nicotine throughout the day are much the same among smokers and those who use smokeless tobacco.
Nicotine withdrawal can lead quitters back to tobacco
- Stopping or cutting back on smokeless tobacco use causes symptoms of nicotine withdrawal much like those smokers get when they quit. Studies have shown that oral snuff users have as much trouble giving up tobacco as cigarette smokers who to quit smoking. Studies also suggest that when regular oral tobacco users can’t use smokeless tobacco, they will often smoke cigarettes or use other ways to get nicotine.
- Withdrawal from nicotine is both physical and mental. Physically, the body reacts to the absence of nicotine. Mentally and emotionally, the user is faced with giving up a habit, which calls for a major, long-term change in behavior. All of these factors must be dealt with to quit and stay that way.
- Those who have used tobacco regularly for a few weeks or longer will have withdrawal symptoms if they suddenly stop or greatly reduce the amount they use. Symptoms usually start within a few hours of the last dip or chew and peak about 2 to 3 days later when most of the nicotine and its by-products are out of the body. Withdrawal symptoms can last a few days to up to several weeks. They will get better every day that you stay tobacco-free.
- Withdrawal symptoms can include any of the following:
- Dizziness (which may last a day or 2 after quitting)
- Depression
- Feelings of frustration, impatience, and anger
- Anxiety
- Irritability
- Trouble sleeping, including trouble falling asleep and staying asleep, and having bad dreams or even nightmares
- Trouble concentrating
- Restlessness or boredom
- Headaches
- Tiredness
- Increased appetite
- Weight gain
- Slower heart rate
These symptoms can lead a person to start using tobacco again to boost blood levels of nicotine and stop symptoms. For information on coping with withdrawal, see the section called “ Dealing with smokeless tobacco withdrawal.”
Quitting smokeless is a little different
- In many ways, quitting smokeless tobacco is a lot like quitting smoking. Both involve tobacco products that contain nicotine, and both involve the physical, mental, and emotional parts of addiction. Many of the ways
to handle the mental hurdles of quitting are the same. But there are 2 parts of quitting that are unique to oral tobacco users:
- There is often a stronger need to have something in the mouth (an oral substitute) to take the place of the chew, snuff, or pouch.
- Mouth sores often start to go away and gum problems caused by the smokeless tobacco often stop getting worse.
There are many reasons to stick it out through withdrawal and quit using smokeless tobacco for good. Health reasons are the most obvious ones. Harmful health effects include:
- Mouth, cheek, and gum cancer
- Cancer in the esophagus (the swallowing tube that goes from your mouth to your stomach)
- Pancreatic cancer
- Possible increase in risk of heart disease, heart attacks, and stroke
- Addiction to nicotine (which can lead to smoking and using other forms of tobacco)
- Leukoplakia (white sores in the mouth that can become cancer)
- Receding gums, gum disease (gums shrink from around the teeth)
- Bone loss around the roots of the teeth
- Abrasion (scratching and wearing down) of teeth
- Cavities and tooth decay
- Tooth loss
- Stained and discolored teeth
- Bad breath
Mouth lesions
- Leukoplakia is a white patch in the mouth that can become cancer. These are sometimes called sores but they are usually painless. Many studies have shown high rates of leukoplakia in the mouth where users place their chew or dip. One study found that nearly 3 out of 4 daily users of moist snuff and chewing tobacco had non-cancerous or pre-cancerous lesions (sores) in the mouth. The longer you use oral tobacco, the more likely you are to have leukoplakia.
- Tobacco can irritate or destroy gum tissue. Many regular smokeless tobacco users have receding gums, gum disease, tooth decay (from the high sugar content in the tobacco), and bone loss around the teeth. The surface of the tooth root may be exposed where gums have shrunken. All this can cause teeth to loosen and fall out.
Heart Disease
- Smokeless tobacco may also play a role in heart disease and high blood pressure. Results from a large American Cancer Society study showed that men who switched from cigarettes to snuff or chewing tobacco had higher death rates from heart disease, stroke, cancer of the mouth and lung, and all causes of death combined than former smokers who stopped using all tobacco products. It’s unclear if the heart disease was caused by the smokeless tobacco products in this study.
- Later studies have found mixed results. Some show a slight increase in heart disease among users of smokeless tobacco. One Indian study that looked at countries where smokeless tobacco use is high found that the risks of heart attack and sudden death were higher in those who used smokeless tobacco, and even higher in those who both chewed and smoked. They also found more high blood pressure and clotting problems in those who used smokeless tobacco. Studies in Sweden found no increase in heart attacks, but snuff (snus) users were more likely to die from their heart attacks than non-users. Other Swedish studies have found that high blood pressure and heart failure are seen at higher rates in snus users compared to peers who do not use tobacco.
- More US studies are needed to identify heart disease related to use of smokeless tobacco.
Carcinogens
- The snuff and chewing tobacco products most widely used in the United States have very high levels of cancer-causing agents (carcinogens) called tobacco-specific nitrosamines. These carcinogens cause lung cancer in animals, even when injected into their blood. There are other cancer-causing agents in smokeless tobacco, too, such as benzo[a]pyrene and other polycyclic aromatic carcinogens. These carcinogens may be why several types of cancer are linked to use of smokeless tobacco (see above list).
How do the risks of using smokeless tobacco compare with cigarette smoking?
- Looking at large numbers of people, smokeless tobacco products are less lethal than cigarettes: They kill fewer people on average than cigarettes. But smokeless tobacco hurts and kills people all the same. Even though smokeless products are marketed as a less harmful alternative to smoking, they can be deadly. Mouth and throat cancer kill far fewer people than lung cancer – a little more than 8,000 per year out of the 42,000 or so that get it. But imagine losing part of your mouth, jaw, face, or neck to cancer. Some people lose their ability to eat or speak. For more on the treatment of mouth and throat cancer, see our document Oral Cavity and Oropharyngeal Cancer.
Social acceptance
- Tobacco use is less socially acceptable now than ever. Chewing and dipping can carry a heavy social price, especially when dating. Bad breath, gum disease, and stained teeth are very unappealing. The spitting you have to do with most smokeless tobacco is not pretty, either. Some employers ban all types of tobacco on their premises. Others won’t hire people who use any form of tobacco.
Cost
- A tobacco habit can cost a lot of money. It isn’t hard to figure out how much you spend on tobacco: Multiply how much money you spend on tobacco every day by 365 (days a year). The amount might surprise you. Now multiply that by the number of years you have been using tobacco and the total will probably shock you.
- Multiply the cost per year by 10 (for the next 10 years) and ask yourself what you would rather do with that much money.
- And this doesn’t include other possible costs, such higher health care and life insurance costs and time away from work due to tobacco-related problems.
Setting an example
- If you have children in your life, you probably want to set a good example for them. When asked, nearly all smokeless tobacco users say they don’t want their children to chew or dip. You can become a better role model for them if you quit now.
Being a slave to the can or pouch
- After long use, many smokeless users start to feel like their lives are being taken over by the can or the pouch. They don’t feel free to live as they’d like because of their tobacco habit. They clearly see how it limits them and causes problems in their lives.
Kicking the tobacco habit offers some benefits that you’ll notice right away and some that will develop over time. These rewards improve most peoples’ day-to-day lives a great deal. Here are just a few:
- Breath smells better
- No more tobacco stains on your face, teeth, or clothes
- Mouth starts to heal – you can eat spicy foods without the burn
- No more looking for empty cans or bottles so you can spit
- Not worrying that people will think less of you for dipping/chewing
- Kissing your spouse or partner before you brush your teeth
Remember, tobacco addiction is mental and physical. For most people, the best way to quit will be some combination of medicine, a method to change personal habits, and emotional support. There are medicines you can try, though they have not been studied as much for quitting smokeless tobacco as they have for smoking. Here are the more common medicines used for quitting tobacco.
Nicotine replacement therapy
- Nicotine replacement is a way to get nicotine without the other harmful chemicals in tobacco. For smokeless tobacco users, nicotine replacement therapy (NRT) has been proven to help reduce craving and withdrawal symptoms. Lack of success in quitting is often related to withdrawal symptoms, which can be reduced with NRT. Together with counseling or other support, NRT can increase the number of smokeless tobacco users who quit.
- The Food and Drug Administration (FDA) has approved these NRT products as effective aids for helping people to quit smoking. None of these products has been FDA-approved specifically to help people quit smokeless
tobacco. Studies are still being done, but many are reporting success using these methods:
- Nicotine gum
- Nicotine patch
- Nicotine lozenges
- Nicotine inhaler
- Nicotine nasal spray
- Nicotine gum, patches, and lozenges can be bought over the counter (without a prescription). Nicotine nasal spray and inhalers are available only with a doctor’s prescription.
- For smokeless tobacco users, certain types of NRT may help more than others. If you look at the way the tobacco is used, nicotine gum and lozenges are most like using smokeless tobacco. They also let you control your dose to help keep nicotine cravings down.
- The nicotine inhaler may not be as useful for smokeless tobacco users, as it’s designed to look and feel like a cigarette. The nicotine patch gives a steady dose of nicotine, but may not help with strong cravings. Still, the patch may be more useful for people who prefer once-a-day convenience. Studies using higher-dose nicotine patches in heavy users of smokeless tobacco have found that the higher doses were more helpful in both reducing withdrawal symptoms and increasing quit rates.
- No matter which type of NRT you choose, make sure to follow the package instructions and don’t use any tobacco, including smokeless tobacco, when using a nicotine replacement.
- NRT products are supposed to roughly match the amount of nicotine you get from NRT to the amount you typically took in through tobacco. It can be more of a challenge to get the dose right for smokeless tobacco users, since NRT products are labeled for smokers.
- In general, a person who uses more than 3 cans of snuff or 3 pouches of tobacco a week is thought of as a heavy user, and would typically use the higher doses of NRT (the dose for heavy smokers). Those who use 2 to 3 cans or pouches per week would usually try the moderate doses, and those who use less than 2 would start with the lowest doses of NRT. If you have decided to try NRT, discuss your dose with your doctor before you quit tobacco.
- To avoid withdrawal symptoms, you want to aim for a nicotine dose fairly close to what you got from snuff or tobacco use. You don’t want to get much more than that, because high doses of nicotine can cause harm. (See the section called “Can you get too much nicotine from NRT?”) If you need more details on NRT products, see our document called Guide to Quitting Smoking.
Getting the most from nicotine replacement
- Nicotine replacement therapy (NRT) only helps with the physical part of withdrawal. It’s not meant to be the only thing you use to quit. NRT works best when it’s used with other quitting aids such as group sessions or counseling. NRT reduces physical withdrawal symptoms so you can focus on coping with the mental and emotional aspects of quitting.
- If you choose to use it, NRT works best if it’s started at the same time you try to quit. Often tobacco users first try to quit on their own, and then decide to try NRT a day or more into quitting. This method does not give you the greatest chance of success, but don’t let this discourage you. There are many options available for quitting.
- You should not use NRT if you plan to keep using any tobacco product. You can get too much nicotine this way.
When can I begin using nicotine replacement therapy?
- You can start using nicotine replacement therapy (NRT) as soon as you throw away your tobacco. You don’t need to wait a certain length of time to put on the patch or start using the gum, lozenge, nasal spray, or inhaler. Double-check this information with the instructions on your chosen method of nicotine replacement, but in general there’s no need to wait to start using NRT.
- Tobacco users who are pregnant or have heart disease should talk to a doctor before using any over-the-counter NRT. You may need a different type of help with quitting, and your doctor may need to see you more often if you use NRT.
Can you get too much nicotine from NRT?
- It’s important to follow the package directions or your doctor’s guidance when using nicotine replacement therapy (NRT). Nicotine overdose is rare, but possible. Even just a bit too much can cause some of the milder symptoms listed below. An overdose can cause death. Overdose is more of a problem with children and pets because of their small size. Nicotine is absorbed through the skin, so you must use, store, and dispose of your NRT safely. Keep new NRT and any used gum or empty bottles, cartridges, patches, etc., safely away from children and pets.
- It would be rare for an adult trying to quit tobacco to get a serious overdose using NRT. But with liquid forms that can absorb quickly through the skin, overdose could happen. That’s why you should not use a heat source (like a heating pad or heat lamp) near your nicotine patch – the extra blood supply could cause more nicotine to absorb. All forms of NRT can be harmful if too much is taken in.
- Here are some symptoms of too much nicotine:
- Headache
- Nausea and vomiting
- Belly pain
- Diarrhea
- Agitation, restlessness
- Fast or irregular heartbeat
- Cold sweat
- Pale skin and mouth
- Weakness
- Tremors (shaking)
- Confusion
- Disturbed vision and hearing
- High blood pressure, which then drops
- Dizziness or faintness (from low blood pressure)
- Seizures
- Fast breathing in early poisoning, breathing may stop later
- Call your Poison Control Center at 1-800-222-1222 and get emergency help if you suspect an overdose. If you’re taking NRT as directed and are still having mild symptoms such as headache, vomiting, diarrhea, or sweating, lower your dose and talk to your doctor.
Prescription medicines
- Prescription drugs are also available to help people quit tobacco. Some can be used along with nicotine replacement therapy (NRT), and some must be started a week or more before you plan to quit. Talk to your doctor if you want to use medicine to help you quit. You will need a prescription for any of these drugs.
Varenicline
- Varenicline (brand name Chantix �) is a prescription medicine taken as a pill twice a day. It works by interfering with nicotine receptors in the brain. It lessens the physical pleasure of taking in nicotine and helps lessen the symptoms of nicotine withdrawal. It must be started at least a week before quitting.
- Varenicline has been found to increase long-term (6-month) success in quitting among smokeless tobacco users. One small study of people who were not trying to quit smokeless tobacco found that a few quit or cut down their tobacco intake while taking varenicline. Other recent studies have shown that smokeless tobacco users taking varenicline were much more likely to quit compared to those taking a placebo (“sugar pill”). Still, more study on this is needed.
- Tell your doctor about any medical conditions and allergies before you start varenicline. Reported side effects have included headaches, nausea, vomiting, trouble sleeping, unusual dreams, gas, and changes in taste. People with heart disease may have a higher risk of heart attacks while taking varenicline. There have also been reports of depressed mood, thoughts of suicide, attempted suicide, anxiety, panic, aggression, confusion, and other changes in behavior or mood in people taking varenicline. People who notice these problems while taking varenicline should contact their doctors right away. Reports of these side effects have been rare, but they can be serious when they do happen. Most people don’t have these emotional or behavioral problems while taking the drug.
- It’s not completely clear if it’s safe to use varenicline along with NRT. More research is needed.
Bupropion
- Bupropion (brand names are Zyban �, Wellbutrin �, or Aplenzin �) is a prescription anti-depressant in an extended-release form that reduces symptoms of nicotine withdrawal. It does not contain nicotine. This drug acts on chemicals in the brain that are related to nicotine craving.
- Bupropion is FDA approved as an aid in quitting smoking, but it’s not clear if it’s useful for smokeless tobacco users. A 2007 study found that it helped reduce cravings and weight gain in people who were trying to quit smokeless tobacco. But in that clinical trial, the group taking bupropion had about the same success rate as the group taking placebo (sugar pills).
- As of 2014, studies have not found bupropion that helpful for people trying to stop using smokeless tobacco.
- Bupropion works best in smokers if they start taking it 1 or 2 weeks before their quit date. The usual dosage is one or two 150 mg tablets per day. Talk to a doctor to find out if this might be an option for you.
- Bupropion can be used alone or with NRT. You should not take it if you have ever had seizures, serious head injury, bipolar (manic-depressive) illness, anorexia or bulimia (eating disorders), cirrhosis, or problems with heavy alcohol use.
Some people can quit without the help of others or the use of medicines. But for many tobacco users, it can be hard to break the social and emotional ties to chewing or dipping while getting over nicotine withdrawal symptoms at the same time. The good thing is, there are many sources of support out there.
Telephone-based help programs
- All 50 states and the District of Columbia offer some type of free, telephone-based program that links callers with trained counselors. These specialists help plan a quit method that fits each person’s unique pattern of tobacco use. Help from a counselor can keep quitters from making many common mistakes that may make it harder to quit.
- Many people find that telephone counseling is easier to use than some other support programs. You don’t have to leave home or get child care, and it’s available on nights and weekends.
- Counselors suggest a combination of methods including local classes, self-help brochures, medicines, and/or a network of family and friends. Research has shown that telephone counseling helps people who are trying to quit smokeless tobacco.
Quit-tobacco programs and support groups
- Joining a support group or taking classes for quitters can help, too. Many workplaces, hospitals, and wellness centers have programs, groups, or classes to help people quit tobacco. They may be led by professionals and focus on information and education, or they may be run by volunteers. Some programs may be set up like classes, while others focus on sharing by members of the group.
- One long-standing peer help program is Nicotine Anonymous �, an open support group that offers a way to find others who are quitting tobacco. It also offers a long-term approach to quitting. (See the “ To learn more” section for contact information.)
- For those who cannot go to classes or support group meetings, there are online support systems as well as phone-based support. There are lots of options, and different types of groups work better for different people. Find one that works for you. See the section “ To learn more” for online and phone programs. Check with your employer, health insurance company, or local hospital to find support groups that fit your needs. Or call us, your American Cancer Society, at 1-800-227-2345.
- What to look for in a tobacco cessation program: Tobacco cessation or quit programs are set up to help users recognize and cope with problems that come up while quitting. This helps the ex-tobacco user avoid common pitfalls of quitting. The programs should also provide support and encouragement in staying tobacco-free. Many programs focus mainly on smokers, but most are open to smokeless tobacco users, too.
- Studies have shown that the best programs include either one-on-one or group counseling. There’s a strong link between how often and how long counseling lasts (its intensity) and the success rate – overall, the more intense the program, the greater the chance of success.
- Intensity may be increased by having more or longer sessions or by increasing the number of weeks over which the sessions are given. So when looking for a program, try to find one that has the following:
- Each session lasts at least 15 to 30 minutes
- There are at least 4 sessions
- The program lasts at least 2 weeks – longer is usually better
Make sure the leader of the group is trained in tobacco cessation.
- Some communities have a Nicotine Anonymous (NicA) group that holds regular meetings. This group applies the 12-step program of Alcoholics Anonymous (AA) to tobacco addiction. This includes attending meetings and following the program. People new to NicA may choose a sponsor to help them through the steps and help them when they are tempted to use tobacco. These meetings are free, though donations are collected to cover expenses. NicA also has web and phone meetings, and offers online support. Often your local American Cancer Society or local health department will sponsor quitting classes, too. Call us for more information.
- Beware of tobacco cessation scams: Not all programs are honest in what they advertise, so be careful. Think twice about any programs that:
- Promise instant, easy success with little to no effort on your part
- Use shots (injections) or pills, especially “secret” ingredients
- Advertise 100% success rate with no ill effects
- Charge a very high fee – check with the Better Business Bureau if you have doubts
- Will not give you references and phone numbers of people who have used the program
Support of family and friends
- Many former tobacco users say a support network of family and friends was very important during their quit attempt. Other people who might be able to offer support and encouragement are your co-workers, family doctor, or dentist.
- Don’t neglect this vital part of quitting. Surround yourself with other people who don’t use tobacco, and tell them about your plans to quit. Warn them that you might not be your usual self for a few days, and ask them to listen and encourage you when you need it. Talk with them about what you need – for instance, patience as you go through cravings, taking your late-night or early-morning phone calls, and plans for doing things where it’s harder to use tobacco. Suggest ways they can help, like going for a walk with you, helping you stay busy, and reminding you that you can do this. If they’ve quit, ask them how they did it and get some tips. Find out what you can count on each friend or family member to do.
- If you have close friends who still use tobacco, ask them not to offer any to you. You’re not asking them to quit themselves, but you might not want to spend a lot of time with those who still use tobacco for the first few weeks after you quit. You could find it hard to be with them without being tempted. But if your plan happens to inspire someone to quit with you, you can help and support each other.
Other tobacco-related and nicotine-containing products have appeared in the past few years. Because they are not marketed to treat nicotine addiction, the FDA doesn’t consider them drugs and doesn’t regulate them. Some may be helpful, but none of these products have been proven to work to help people quit using tobacco.
Non-tobacco snuff products
- These are sold in grocery and convenience stores, online, or by mail order. They are packaged like moist snuff in a tin and come in different flavors. They are made from plants or herbs such as tea, clover, mint leaves, kudzu, or alfalfa. Some have added flavors and moisteners like glycerin. At least one contains an herb called guarana, which has quite a bit of caffeine in it.
- Non-tobacco snuffs can be used alone or mixed with regular snuff as a person is trying to cut down on tobacco. They are generally considered safe as long as you’re not allergic to anything in them, but they have not been reviewed by the FDA and there’s not much research on whether they help people quit. One study that used mint snuff as a substitute found that it helped reduce cravings in smokeless tobacco users who were trying to quit. But those who used the mint snuff were no more likely to quit tobacco than those who didn’t. If you choose to try a non-tobacco snuff, check the ingredient list to see what you are getting.
Hypnosis
- Hypnosis methods vary a great deal, which makes hypnosis hard to study as a way to quit tobacco. For the most part, reviews that looked at controlled studies of hypnosis to help people quit smoking have not supported it as a quitting method that works. As a way to quit using smokeless tobacco, hypnosis has been studied even less. Still, it might be useful for some people. If you’d like to try it, ask your doctor to recommend a good licensed therapist who does hypnotherapy.
Acupuncture
- This method has been used for quitting tobacco, but there’s little evidence to show that it works. It involves putting small needles into the skin, usually around the ears. For a list of local doctors who do acupuncture, contact the American Academy of Medical Acupuncture online at www.medicalacupuncture.org, or call 323-937-5514.
Low-level laser therapy
- This technique, also called cold laser therapy, is related to acupuncture. Despite claims of success by some cold laser therapy providers, there’s no scientific evidence that this helps people stop using tobacco.
Tobacco deterrents
- These include over-the-counter products that change the taste of tobacco, “quitting diets” that are supposed to curb nicotine cravings, and combinations of vitamins. There’s little scientific evidence to support claims that any of these methods work.
Herbs and supplements
- There’s little scientific evidence to support the use of homeopathic aids and herbal supplements as methods to help a person quit tobacco. Because they are marketed as dietary supplements (not drugs), these products don’t need FDA approval to be sold. This means that the manufacturers don’t have to prove they work, or even that they’re safe.
- Be sure to look closely at the label of any product that claims it can help you quit tobacco. Dietary supplements and homeopathic remedies have no proven track record of helping people quit tobacco.
Nicotine lollipops and lip balms
- In the past, some pharmacies made a product called a nicotine lollipop. These lollipops often contained a product called nicotine salicylate, which is not approved by the FDA for pharmacy use. The FDA has warned pharmacies to stop selling nicotine lollipops and lip balm, calling the products “illegal.” The FDA also said “the candy-like products present a risk of accidental use by children.”
- Other tobacco cessation products like these that do not use nicotine salicylate may be legal if they are prescribed by a doctor. But they still pose a risk for children and pets if they are not well-labeled, stored safely, and disposed of where children and pets cannot get them.
Tobacco lozenges, strips, and pills
- Lozenges, sticks, strips, and pills that contain tobacco are now being marketed as other ways for smokers to get nicotine in places where smoking is not allowed. They are not sold as ways to quit tobacco. The FDA has ruled that these are types of smokeless tobacco, not aids to quit smoking or wean off tobacco. There’s no reason to think these products would have fewer health risks than more common forms of smokeless tobacco.
Snus
- Swedish snus has been touted by some people as a safer way to use tobacco, and even as a way to quit smoking cigarettes. Snus made in Sweden is a type of moist snuff that is reported to have lower levels of tobacco-associated nitrosamines (TSNAs), a potent cancer-causing agent in tobacco products. Lower TSNA levels may mean less risk of cancer, but there are still TSNAs and other carcinogens in Swedish snus.
- American versions of snus contain varying amounts of TSNAs depending on brand and region of the United States. Levels of TSNAs are not regulated in American snus, nor is there a requirement for labeling about this carcinogen. And, as with Swedish snus, there are other carcinogens besides TSNAs. To date, snus has not been tested in controlled clinical trials as a way to stop smoking. Snus contains tobacco, so it’s not helpful if your goal is to quit; it’s as addictive as any other form of tobacco. American snus has not been proven safer than the more common forms of smokeless tobacco.
- For more on snus, see our document called Smokeless Tobacco.
- Before you sign up for a tobacco cessation class or program, you may wonder about its success rate. Success rates are hard to figure out for many reasons. First, not all programs define success in the same way. Does success mean that a person is not using tobacco at the end of the program? After 3 months? 5 months? 1 year? If a program you’re considering claims a certain success rate, ask for more details on how success is defined and exactly how they were able to confirm the rate.
- The truth is that a good program to help you quit tobacco may give you more of an edge than trying to quit on your own. But like other programs that treat addictions, they often have fairly low success rates. That doesn’t mean they are not worthwhile, or that you should be discouraged. Your own success in quitting and staying tobacco-free is what really counts, and you have some control over that. Even if you don’t succeed the first few times, keep trying. You can learn from your mistakes so that you’ll be ready for those pitfalls next time.
Tobacco users often say, “Don’t tell me why to quit, tell me how.” There’s no one right way to quit, but there are some things that can help you quit for good. The 4 key factors are:
Only you can decide you want to quit using tobacco. Others may want you to quit, but the real commitment must come from you.
Think about why you want to quit
- Are you worried that you could get a tobacco-related disease?
- Do you really believe that the benefits of quitting outweigh the benefits of continuing to use tobacco?
- Do you know someone who has had health problems because of tobacco use?
- Are you ready to make a serious try at quitting?
List your reasons for quitting
- Tobacco users have many reasons for wanting to quit. But what motivates you to quit may not be the same as what motivates others. Think about making a list of the reasons you want to quit – one you can review later if you’re feeling tempted. The list might include some or all of the following, but be sure to add your own reasons:
- I want to be healthier.
- I already have problems with my gums/teeth, and I don’t want them to get worse.
- I don’t want to spend my money on this.
- I can’t chew/dip at work/school.
- I want to be able to go to a movie/mall/ballgame without worrying about it.
- I want to prove I can do it.
- I don’t want it to control me.
- The people I care about don’t like it, and want me to quit.
- I want to set a good example for the kids.
If you’re thinking about quitting, setting a date and deciding on a plan will help move you to the next step.
Once you’ve decided to quit, you’re ready to pick a quit date. This is a very important step. One study of smokeless tobacco users who were offered nicotine replacement therapy found that even in those who did not plan to quit, picking a Quit Day and then quitting on that day led to much better success staying quit 6 months later compared to those who gradually reduced their use of tobacco.
Pick a day in the next month as your Quit Day. Picking a date too far away gives you time to rationalize and change your mind. But you want to give yourself enough time to prepare and come up with a plan. You might choose a date that has a special meaning, like a birthday or anniversary, or the date of the American Cancer Society Great American Smokeout (the third Thursday in November each year). Or you might want to just pick a random date. Circle the date on your calendar. Make a strong, personal commitment to quit on that day.
Plan for your prescriptions
- If you are thinking of using a prescription drug, you will need to talk with your doctor about getting it in time for your Quit Day. Talk with your doctor about exactly how to use the medicine and when to start taking it. If you’re going to use a prescription drug, put a note on your calendar to remind you when to start taking it.
Cut down on how much you use
- One way to cut back before quitting is to cut down on the number of times or the amount you dip or chew each day. By doing this, you slowly reduce the amount of nicotine in your body. Try cutting back to half of your usual amount before you quit. If you usually carry your tin or pouch with you, try leaving it behind. Carry something else to put in your mouth instead.
Cut back on when and where you use
- You can also try cutting back on when and where you dip or chew. This gives you a chance to notice when your cravings are the worst. It helps you decide on a game plan if you know what triggers your cravings. Again, once you’ve decided not to use tobacco at a certain place, leave your pouch or tin at home when you go there. Try your substitutes instead. (See the section called “Some steps to help you prepare for your Quit Day.”)
Put off using tobacco when you have a craving
- Go as long as you can without giving into a craving. Start by trying for at least 10 minutes, then longer and longer as you near your Quit Day. Pick your 3 worst triggers and stop dipping or chewing at those times. This will be hard at first, but practice will make it easier.
- Quitting tobacco is a lot like losing weight. It takes a strong commitment over a long time. Users may wish there were a magic bullet – a pill or method that would make quitting painless and easy. But there’s nothing like that. Nicotine substitutes can help reduce withdrawal symptoms, but they work best when used as part of a quitting plan that addresses the physical, mental, and emotional parts of quitting.
Some steps to help you prepare for your Quit Day
- Pick your Quit Day and mark it on your calendar.
- Tell friends, family, and co-workers about your Quit Day, and let them know how they can help.
- Get rid of all the tobacco in your home, car, and workplace the night before your Quit Day.
- Stock up on other things to put in your mouth – for instance, sugarless gum, carrot sticks, beef jerky, cinnamon sticks, and/or sugarless hard candy.
- Decide on a plan. Will you use nicotine replacement therapy or other medicines? Will you go to a class or program? If so, sign up now.
- Consider seeing your doctor or dentist. Have them check your mouth, and discuss your plan for quitting with them.
- Set up a support system. This could be a group program, Nicotine Anonymous, or friends or family members who have quit and are willing to help you.
- Ask family and friends who use tobacco not to use it around you or leave it out where you can see it.
- If you are using varenicline or bupropion, take your dose each day leading up to your Quit Day.
- Make a list of your “triggers” – situations, places, or feelings – that make you more likely to use tobacco. Being aware of these can help you avoid them or at least be ready for them.
- Think back to your other attempts to quit. Try to figure out what worked and what didn’t.
Successful quitting is a matter of planning and commitment, not luck. Decide now on your own plan. Some options include joining a tobacco cessation class, calling a cessation support line, going to support meetings, using nicotine replacement or other medicines, online support, and using self-help materials such as books and pamphlets. For the best chance of success, your plan should include 2 or more of these options.
On your Quit Day
- Don’t use tobacco of any kind. This means none, not even a pinch!
- Stay busy – try walking, short bursts of exercise, or other activities or hobbies.
- Keep substitutes handy to put in your mouth.
- Drink lots of water and juices.
- Start using nicotine replacement if that’s your choice.
- Call a quit support line, go to a quit class, or follow your self-help plan.
- Avoid situations where the urge to dip or chew is strong.
- Avoid people who are using tobacco.
- Avoid alcohol. It can weaken your resolve to quit
- Think about how you can change your routine. Sit in a different chair at home, drive a new route to work, or choose foods and drinks that make tobacco taste bad.
Staying quit is the final, longest, and most important stage of the process. You can use the same methods to stay quit as you did to help you through withdrawal. Plan ahead for those times when you may be tempted to use tobacco. Think about other ways to cope with these situations.
More dangerous, perhaps, are the unexpected strong desires to use tobacco that crop up months or even years after you’ve quit. Rationalizations can show up then, too. To get through these without relapse, try these:
- Review your reasons for quitting and think of all the benefits to your health, your finances, and your family.
- Remind yourself that there’s no such thing as just one chew or dip.
- Ride out the desire. It will go away, but don’t fool yourself into thinking you can have just one dip or chew.
- Avoid alcohol. Drinking lowers your chance of success.
- If you’re worried about gaining weight, put some energy into planning a healthy diet and finding ways to exercise and stay active.
What if you slip and use tobacco after your Quit Day?
- What if you do use tobacco? Here’s the difference between a slip and a relapse: a slip is a one-time mistake that’s quickly corrected. A relapse is going back to your former habit. You can use the slip as an excuse to go back to using tobacco, or you can look at what went wrong and renew your commitment to staying away from tobacco for good.
- Even if you do relapse, try not to get too discouraged. Very few people are able to quit for good on the first try. In fact, it takes most people several tries before they quit for good. What’s important is figuring out what helped you in your attempt to quit and what worked against you. You can then use this information to make a stronger attempt at quitting the next time. Learn from your mistakes, and don’t give up!
Weight gain
- It’s well known that smokers often gain weight when they quit, but fewer studies have been done on people quitting smokeless tobacco. Still, findings suggest that people who quit smokeless tobacco have some risk of weight gain. Don’t let this stop you!
- You’re more likely to succeed in quitting if you deal with quitting tobacco first, and then later take steps to lose weight. While you are quitting, try to focus on ways to help you stay healthy, rather than on your weight. Stressing about your weight may make it harder to quit. Eat plenty of fruits and vegetables and limit fat. Be sure to drink plenty of water, and get enough sleep and regular physical activity.
Try walking
-
Walking is a great way to be physically active and increase your chances of staying quit. Walking can help you by:
- Reducing stress
- Burning calories and toning muscles
- Giving you something to do instead of thinking about tobacco
- A pair of comfortable shoes is all most people need for walking. And most people can do it pretty much anytime. You can use these ideas as starting points and come up with more of your own:
- Walk around a shopping mall
- Get off the bus one stop before you usually do
- Find a buddy to walk with during lunch time at work
- Take the stairs instead of the elevator
- Walk with a friend, family member, or neighbor after dinner
- Push your baby in a stroller
- Take a dog (yours or maybe a neighbor’s) for a walk
- Set a goal of at least 2 � hours of moderate intensity physical activity spread throughout each week. But if you don’t already exercise regularly, please check with your doctor before you start. If you’d like to learn more, please see our American Cancer Society Guidelines on Nutrition and Physical Activity for Cancer Prevention.
Stress management
- Tobacco users often mention stress as one of the reasons for going back to using tobacco. Stress is part of life for everyone, whether or not they use tobacco. The difference is that tobacco users have come to use nicotine to help cope with stress and unpleasant emotions. When quitting, you have to learn new ways to handle stress. This can be tough, especially during the first few days. Nicotine replacement can help for a while, but over time you will need other methods.
- As mentioned before, physical activity is a good stress reducer. It can also help with the short-term sense of depression or loss that some tobacco users have when they quit. There are also stress-management classes and self-help books. Check your community newspaper, library, or bookstore.
- Spiritual practices involve being part of something greater than yourself. For some, that includes things like religious practices, prayer, or church work. For others, it may involve meditation, music, being outside in nature, creative work, or volunteering to help others. Spirituality can give you a sense of purpose and help you remember why you want to stay quit.
- The spiritual practices of admitting that you can’t control your addiction and believing that a higher power can give you strength have been used with much success to deal with other addictions. These practices, along with the fellowship of others on a similar path, are a key part of 12-step recovery programs. These same principles can be applied to quitting tobacco.
- Think about how you can deal with stress and not use tobacco. Look at the resources around you and plan on how you will handle stress when it comes your way.
It’s hard to give up tobacco. But you can quit! Many organizations offer free information, counseling, and other services focusing on how to quit and where to go for help. Other good resources to ask for help can include your doctor, dentist, local hospital, or employer. You can call us at 1-800-227-2345 or visit us online at www.cancer.org. There are also other groups listed below that can help you.
National organizations and websites*
- Kill the Can
- Website: www.killthecan.org
- Online information, encouragement, and support for those committed to quitting smokeless tobacco
- Nicotine Anonymous (NicA)
- Toll-free number: 1-877-879-6422 (1-877-TRY-NICA)
- Website: www.nicotine-anonymous.org
Additional Cessation Information
- Impacts of Tobacco (PowerPoint)
- American Cancer Society: Stay Away from Tobacco
- US Food and Drug Administration: Smoking Cessation Products
Nicotine Replacement Therapies (NRT) Coverage
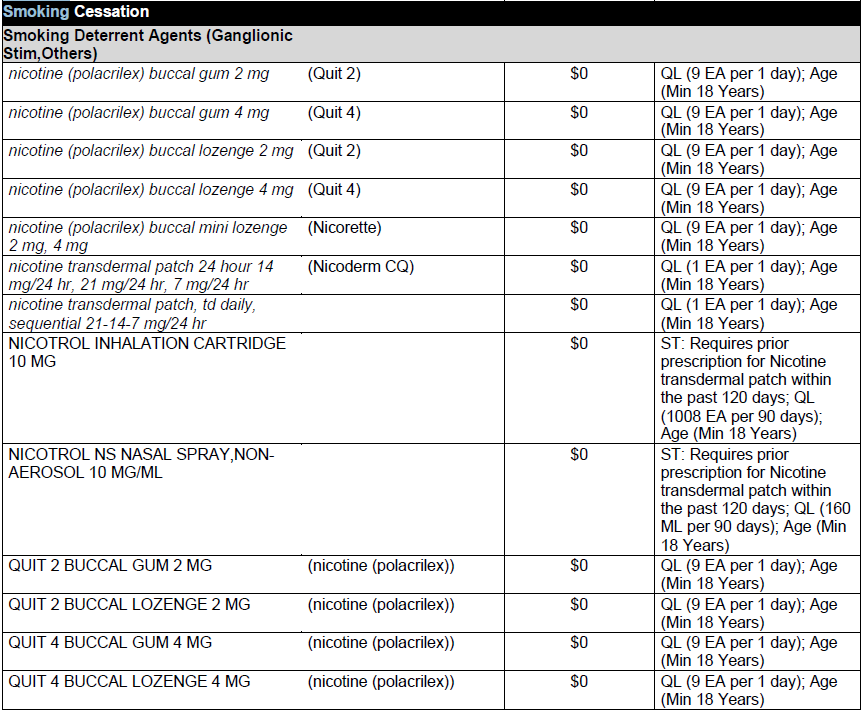
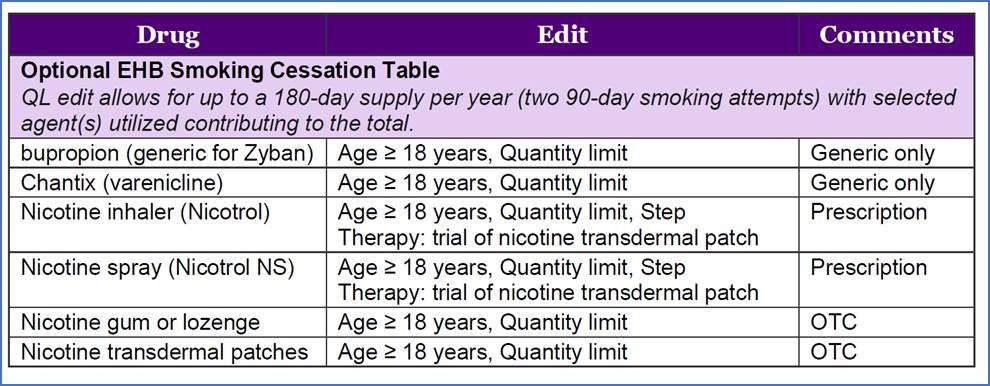
As of July 1, 2022 the State of Maine has elected to cover certain smoking cessation products according to the guidelines in the ACA/EHB Zero Dollar Copay Preventive Medication List. According to the guidelines, two 90-day smoking attempts (180-day supply per year) are allowed for members. Age limitations, Step Therapy, and Quantity limits apply.
Below is an excerpt of the MedPerform Medium Formulary in regards to smoking cessation coverage and limitations.